Scoliosis is a condition in which the spine has an abnormal sideways curvature, typically in a “C” or “S” shape. Scoliosis most commonly occurs in the upper and mid-back (the thoracic spine).
There are a few different types of scoliosis. If there is an underlying neurologic cause (such as cerebral palsy or muscular dystrophy), the condition is called neuromuscular scoliosis. In congenital scoliosis, segments of the spine either fail to segment or parts fail to form in utero. However, the most common type of scoliosis is idiopathic, which means that there is not a known cause for the curvature.
Idiopathic scoliosis is most commonly discovered and treated in adolescent patients. When discovered early, idiopathic scoliosis can often be treated without surgery, so proper evaluation by a qualified specialist is important.
What Is adolescent idiopathic scoliosis?
Adolescent idiopathic scoliosis is the most common type of idiopathic scoliosis, comprising more than 80% of all patients with idiopathic scoliosis. The adolescent age group is defined as ages 10-18, and typical curve types are C shape or S shape in the coronal plane. The spine rotates as it curves, resulting in rib hump deformity, shoulder imbalance, or waist asymmetry seen on physical examination. Scoliosis affects girls more than boys at a ratio of 8:1.
Idiopathic scoliosis is thought to be present in 2% to 3% of adolescents. One in 500 of these adolescents will require active treatment, and only one in 5,000 will progress to the degree that surgery is indicated. The cause of idiopathic scoliosis is unknown, but approximately 30% of patients have a significant family history of scoliosis.
Symptoms
Most of the time, the scoliosis is asymptomatic and is discovered in routine physical examination, school screening, or is noticed by the patient or family.
Some curves do, in fact, cause pain. In that situation, other potential causes of pain need to be explored. It can never be assumed that scoliosis is the cause. Progression of the curve tends to occur in the secondary growth spurt around the time of menarche.
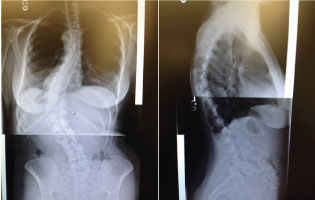
Imaging to evaluate scoliosis
After a thorough examination, standardized 36-inch PA and lateral standing scoliosis films are necessary to evaluate adolescent idiopathic scoliosis. Even highly trained scoliosis specialists can measure curves differently and arrive at different numbers. The most qualified specialist should determine the actual curve measurement and assess all subsequent radiographs to try to determine whether progression is actually occurring.
Radiation exposure is a concern for all female patients, particularly growing adolescents. Proper imaging minimizes the need to repeat films. It is important to limit the number of films a patient receives over the course of treatment because all x-ray exposure is cumulative. X-rays often show structural changes including asymmetric growth of the apical vertebrae, a keystone feature of idiopathic scoliosis. Structural vertebral changes indicate that the deformity was present prior to cessation of growth.
Treatment for adolescent idiopathic scoliosis
Bracing is the only proven non-operative treatment that can prevent progression of scoliosis and, in some rare cases, improve the curve. Bracing is only effective if there is growth remaining and in curves between 25 and 40 degrees. The location of the curve can sometimes determine whether a brace is going to be effective. The window of opportunity is lost when growth is completed.
There is no scientific proof that alternative treatments, such as, physical therapy, chiropractic care, or yoga have any value in treating scoliosis in a growing child. Alternative treatments can be utilized if desired by the patients or their families to relieve symptoms after the patient reaches skeletal maturity. However, these techniques should not be used to treat the curvature in the hopes that it will improve the scoliosis.
Surgery for scoliosis
Surgery is reserved for thoracic curves greater than 50 degrees. Thoracolumbar and lumbar apex curves are sometimes treated when they are less than 50 degrees. Severe hypo-kyphosis or thoracic lordosis also indicate surgery because of their significant effect on pulmonary function.
Current surgical techniques include pedicle screw segmental fixation to straighten and de-rotate the spine. It is important to limit the fusion levels to the major curve and maintain flexibility in the lumbar spine. Modern scoliosis surgery techniques allow for aggressive correction and de-rotation of the deformity, often allowing the surgeon to address only the major curve, leaving the compensatory lumbar curves alone and maintaining important lumbar spine flexibility.
Over the years, several alternatives to the posterior approach have been introduced for scoliosis surgery. However, the majority of surgeons around the world still regard the open posterior approach as the best option for the treatment of idiopathic scoliosis. The reasons are simple: posterior correction is well-tolerated by patients and has a low complication rate, a high patient satisfaction rate, and a high long-term fusion rate.

A small minority of surgeons are attempting correction through a more minimally invasive (MIS) posterior approach through multiple small incisions. This involves tunneling under the skin to reach the joints in intermediate sections that are not directly exposed. Instrumentation is placed under the skin with x-ray assist. The MIS approach to adolescent or adult scoliosis has not been proven to be more effective in the treatment of scoliosis and has been linked to poor correction of spinal alignment. With any change in surgical technique, it may take 5-10 years to determine if fusion rates and patient outcomes are consistent with the standard approach. While many new surgical techniques are introduced as "the answer" to a problem, longer-term evidence reveals that these new techniques are only appropriate for very limited indications.
Our major concerns with MIS approach idiopathic scoliosis are two-fold:
- Radiation exposure: No one knows the long-term effects of prolonged X-ray exposure to growing children required with MIS techniques.
- It will take years, maybe decades, to know what the fusion rates and re-operation revision rates will be. Current well established posterior fusion techniques result in high fusion rates, low complication, high rates of curve correction with maintenance of sagittal and coronal balance. This is a well-tolerated procedure with excellent outcomes in this patient population. It is the technique used worldwide by most physicians specializing in treatment of scoliosis.
What about scoliosis treatment in adults?
The major difference in treating an adult and adolescent with idiopathic scoliosis is the degeneration of the lumbar spine in adulthood. Adult scoliosis patients often have painful conditions, including disc degeneration, spinal stenosis, and degenerative or rotatory spondylolisthesis, below the major curves. Sometimes, the major curves themselves can cause symptoms with age. Traditionally, age groups are divided as adolescent (10 to 18 years) and adult (18 and older). With that said, the course of surgical treatment is nearly identical to the adolescent group for patients up to age 30.
In the adolescent patient, curve progression determines whether surgery is recommended; however, curve progression alone is rarely the indication in adult patients over 30. Typically, surgery is only recommended if the curve is progressing at a rate that could eventually cause a serious medical condition, like restrictive lung disease.
Adult patients that experience increasing lower back pain or decreasing ability to stand upright or sit upright unsupported may elect to have surgery. In this select group, if their disability is progressive, it may be beneficial to treat them at a younger age when there is a lower risk of complications. Adult spinal deformity surgery for patients aged 60 and up has a much higher complication rate. Patients with the most significant disabilities and symptoms are the ones that gain the most benefit from surgery.
Idiopathic scoliosis only affects only 2 to 3% of the population. The window of opportunity for nonoperative brace treatment in the growing child is clear and that window of opportunity closes at skeletal maturity. Early diagnosis is the key to successful nonoperative management.
Scoliosis treatment in Austin, TX
The spinal deformity experts at Austin Spine offer a variety of nonsurgical and surgical treatment options for scoliosis, which are tailored to the needs of the patient. Early detection, treatment, and monitoring are important for adolescent patients with idiopathic scoliosis. To learn more about our scoliosis treatment options or schedule an appointment with one of our specialists, please call our office at (512) 347-7463.